I received a call at 4 AM to check on a patient as the circulating rapid response nurse. He was two days post-op with a perforated appendix, and had been clinically stable.
The nurse explained that he had become more lethargic, tachypneic, tachycardic over the last four hours, and was now unresponsive.
I took one look and knew that this patient was in trouble!
He was pale, cold and diaphoretic. The last blood pressure red 158/90. I asked when the last blood pressure was taken. She replied four hours ago. After a quick recheck it was now 68/30.
Realizing that this patient was in septic shock and needed a central line, he was emergently transferred to ICU where he was intubated, started on three vasopressors and IV antibiotics. All to no avail because he died the next day (See my past blog “I See Dead Patients”)
How to Be a Superhero!
Had this nurse recognized the EARLY but subtle signs of sepsis, this death could have likely been prevented by the needless progression to irreversible septic shock.
This is how a nurse who is able to clinically reason by recognizing which patients are at risk as well as recognize EARLY signs of sepsis can be a superhero and prevent an adverse outcome and even preventable patient death! (See past blog on nurse vigilence)
Patient safety is not just about keeping the bed in a low position and putting the side rails up! The ability to THINK like a nurse by being able to clinically reason is ultimately a patient safety issue that must be a priority for every nurse educator to strengthen and develop in every student before graduation! (See past blog on developing nurse thinking)
Sepsis Stats
Sepsis is a KILLER that continues to be a growing problem in health care settings across the country. Just how big? The following statistics are sobering. According to the Centers for Disease Control (CDC):
- Sepsis is a leading cause of death and hospitalization in the United States
- Sepsis is the most common complication after any invasive procedure and is responsible for more deaths than heart disease in the United States.
- Sepsis affects more than 750,000 individuals annually, with 33% of sepsis cases resulting in death
- Sepsis occurs in just 10% of U.S. hospital patients, but it contributes to as many as half of all hospital deaths
- 30% of deaths or serious health problems stemming from sepsis are considered preventable.
Recognizing Sepsis
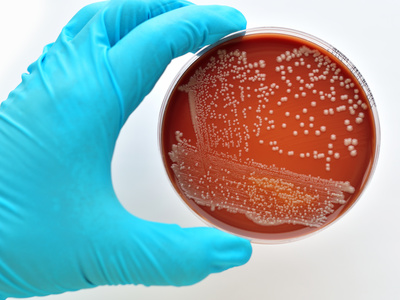
Sepsis begins as a localized infection that goes throughout the body causing a systemic inflammatory response syndrome (SIRS).
Though infection, inflammation, and immunity are separate concepts, they are interrelated and each must be DEEPLY understood and applied to acquire the deep knowledge that is required to think critically and recognize sepsis EARLY, before it progresses to the life-threatening complication of septic shock (See past blog on looking for “Jason”).
To go deeper and explore the pathophysiology of sepsis and inflammation, though a physicians database emedicine.medscape.com is my favorite online resource. Here is the link to sepsis/SIRS.
Identifying SIRS
SIRS is nonspecific and can be caused by ischemia, inflammation, trauma, infection, but does manifest most commonly as a bacterial infection.
The nurse must understand physiology to be able to state the WHY and clinical significance of the following symptoms that identify SIRS which is defined as 2 or more of the following:
-
Fever of more than 38°C (100.4°F) or less than 36°C (96.8°F)
-
Heart rate of more than 90 beats per minute
-
Respiratory rate of more than 20 breaths per minute
-
Abnormal white blood cell count (>12,000/µL or < 4,000/µL or >10% immature [band] forms)
Labs that are ALWAYS Relevant
In addition to WBCs, the other labs that are always relevant and must be noted by the nurse in sepsis/SIRS include:
- Neutrophil %
- ALWAYS RELEVANT for same reason as WBCs. They are the most common leukocyte and their role as a FIRST RESPONDER to any bacterial infection within several hours is always relevant.
- The more aggressive or systemic the infection, the higher the percentage of neutrophils and WBCs. Immature neutrophils (bands) greater than 8 are also clinically significant and must be clustered with WBC and neutrophils to determine if sepsis is a clinical concern.
- Bands
- Immature neutrophils that are elevated in sepsis as the body attempts to fight infection and releases these prematurely. If elevated, it’s a clinical RED FLAG in the context of sepsis. If elevated to >8, it is considered a “shift to the left,” which indicates impending sepsis.
- Lactate
- Remember Krebs cycle and lactic acidosis in A&P due to anaerobic metabolism? GOLD STANDARD lab to trend with any shock state, especially sepsis! Elevated levels correlate with higher likelihood of dying. For example, in septic shock, a level >4 reflects a 28 percent mortality. Lactate builds up within the serum and can be seen as a marker of strained cellular metabolism.
Put it All Together!
In last week’s blog, I discussed how a salient scenario and case study can bring needed context to content. Here is a simple scenario that can help contextualize this essential content on SIRS and sepsis to clinical practice:
Patient Scenario:
Jimmy Jones is a 38-year-old African-American male with a relevant history of C-4 quadriplegia 2 years ago secondary to a car accident. He was seen today in outpatient clinic for a wound check for a baseball-sized stage 4 decubiti on his coccyx that he developed 6 months ago. He developed chills and a fever yesterday. His current VS: T: 100.5 (o) P: 94 R:20 BP: 90/52 O2 sat: 99% RA. He has a large amount of yellow/green drainage on the dressing and the drainage has a strong odor.
The nurse must reflect and answer the following clinical reasoning questions:
- What data is RELEVANT from patient scenario?
- Clinical significance?
Current VS:
| T: 101.2 (oral) |
| P: 110 (regular) |
| R: 22 (regular) |
| BP: 92/50 |
| O2 sat: 95% RA |
Complete Blood Count (CBC:) |
Current: |
| WBC (4.5–11.0 mm 3) | 12.9 |
| Hgb (12–16 g/dL) | 11.8 |
| Platelets (150–450 x103/µl) | 188 |
| Neutrophil % (42–72) | 89 |
| Band forms (3–5%) | 1 |
Basic Metabolic Panel (BMP:) |
Current: |
| Sodium (135–145 mEq/L) | 135 |
| Potassium (3.5–5.0 mEq/L) | 4.2 |
| Glucose (70–110 mg/dL) | 95 |
| Creatinine (0.6–1.2 mg/dL) | 0.4 |
Lactate (<2.0) 1.9
The nurse must reflect and answer the following clinical reasoning questions of these lab results:
- What lab values are RELEVANT?
- Clinical significance?
- What clinical data confirms the presence of SIRS?
In Closing
It is imperative to embrace a comprehensive approach to patient safety and recognize that thinking like a nurse through an emphasis of clinical reasoning applied to practice is the foundation of nursing education.
How well prepared are your students to recognize the early signs of sepsis before it progresses to septic shock? Do they truly understand the pathophysiology and the rationale for clinical data that is abnormal?
This content must not just be memorized, but deeply understood and applied in the clinical setting.
When students have a deep and applied understanding of clinical reasoning, they are prepared to think like a nurse and can literally be a superhero who can and will save and rescue patient lives from the most likely or worst possible complications including sepsis!
What do you think?
How are you preparing students to clinically reason that will prevent failure to rescue?
Comment below and let the conversation begin!
Keith Rischer – Ph.D., RN, CCRN, CEN
As a nurse with over 35 years of experience who remained in practice as an educator, I’ve witnessed the gap between how nursing is taught and how it is practiced, and I decided to do something about it! Read more…
The Ultimate Solution to Develop Clinical Judgment Skills
KeithRN’s Think Like a Nurse Membership
Access exclusive active learning resources for faculty and students, including KeithRN Case Studies, making it your go-to resource.