Current Nursing Student Outcomes
Despite recently rising NCLEX pass rates nationwide (1), we’re seeing a troubling trend: new graduates who lack entry-level clinical judgment competency (2) and are not successfully transitioning to clinical practice with up to one-third of our new nurses leaving the profession entirely after two years (3).
Though there are many variables for these findings, it is an opportunity to reflect on how nursing is taught to prepare them for practice and ask:
Are we teaching nursing in a way that reflects how it is actually practiced?
To answer, ponder the following questions I have asked myself for many years during my journey as an experienced nurse who entered nursing education.
- Does a precisely worded 3-part NANDA diagnosis statement on a multiple-page care plan reflect how nurses actually think at the bedside?
- Do multiple-choice exams, even the NCLEX, prepare students for the open-ended, high-stakes decisions of real-world practice?
- Should we teach students a clinical judgment model that relies on academic language like “cues” and “hypotheses”, words that are rarely, if ever, used by nurses in practice?
- Are we consistently using active learning in our classrooms, such as using authentic case studies to practice the open-ended thinking of practice?
Developing Clinical Judgment with Teaching Frameworks
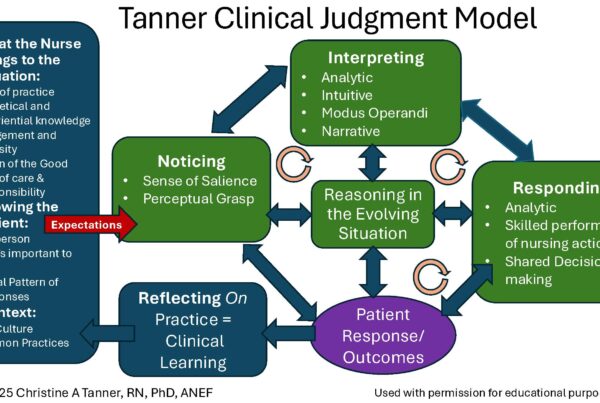
Although there is a greater emphasis on clinical judgment than ever before in nursing education, the majority of nursing programs do not use a theoretical model to teach clinical judgment. Of those that do, Tanner’s Clinical Judgment Model (CJM) is the most common (4).
By intentionally adopting a CJM such as Tanner’s (5), programs can transition from fragmented strategies to a cohesive, practice-ready curriculum, thereby fulfilling nursing’s purpose of preparing graduates for safe practice (4).
Over the years with KeithRN, I’ve worked to develop a series of open-ended reflection questions in our case studies and clinical tools based on Tanner’s model.
To make Tanner’s model easier to remember for students and provide practice-based insights, I recently developed a tool that makes each of Tanner’s clinical reasoning steps begin with “R”, the 6 R’s of Clinical Reasoning, but adding a crucial step of “risk recognition” I used in practice, visible so students can incorporate this thinking process into their practice as a new nurse.
Here’s the teaching framework of the 6 R’s with an essential question(s) students or new nurses need to reflect on and answer:
New Teaching Framework: The 6 R’s of Clinical Reasoning
 1. RECOGNIZE Relevant Data (Noticing)
1. RECOGNIZE Relevant Data (Noticing)
- What is the most important clinical data you noticed?
2. RELATIONSHIPS Identified (Interpreting)
- What does the most important data mean?
- What clinical data has a relationship (can be connected)?
For this step, I broke down the interpretation process into two essential steps. By first reflecting on what the data means or its clinical significance, can the relationships of the clinical data be recognized.
3. RESPOND to Current Priority (Responding)
- What is the current nursing priority?
- What will be your priority nursing intervention(s)? State rationale and expected outcome(s).
4. RISKS & RED Flags Identified (not made visible in Tanner’s CJM)
- What can you do to prevent this complication from developing (if possible)?
- What clinical data (red flags) would help you identify this complication early?
5. RE-EVALUATE Patient’s Response (Reflecting-in-action)
- Was the patient’s response to the plan of care expected or unexpected?
- What is the current nursing priority? Has it changed?
- What nursing intervention is needed now—and why?
6. REFLECT & REFINE Thinking (Reflecting-on-action)
- Which one (or more) of the six R’s of clinical reasoning do you need to strengthen to improve your clinical reasoning?
- What will you do to strengthen your future clinical reasoning skills? (Create a plan of action)
Free Download
 I have created a bundle of resources that any educator can download and use in their program to strengthen and complement how clinical judgment is taught:
I have created a bundle of resources that any educator can download and use in their program to strengthen and complement how clinical judgment is taught:
Educator’s User Guide. Concise summary of the “why” and “how” to implement in your teaching.
Educator Worksheet. Summary sheet of each “R” and additional reflection questions to ask students.
Student Worksheet. Each “R” has an essential reflection question that must be answered that captures the essence of a practice-based careplan and way of thinking, plus a student reflection summary.
My Story
As a nurse in critical care and emergency settings, I quickly learned that patient status can change quickly. This taught me to anticipate and recognize risk before it turns into a life-threatening crisis.
I began to ask myself with every patient I cared for:
“What is the worst possible or most likely complication this patient could develop?”
Then I’d ask:
“What red flags would help me identify it early?”
For instance, if I were caring for a stable post-op patient, pain might be the primary problem, but I knew I needed to watch for sepsis. I’d stay alert to subtle signs of this potential problem early… a trending elevated heart rate, softening blood pressure, a rise or drop in temperature, signs that could signal early decline.
Later, as I transitioned into education after 25 years of practice, I saw a concerning gap: we weren’t teaching students to think this way. Our teaching models focused on recognizing current priorities, but didn’t explicitly address potential risk recognition. See comparison table below.
Clinical Reasoning Teaching Framework Comparison Table
| 6 R’s of Clinical Reasoning | The Nursing Process | Tanner’s CJM | NCSBN CJMM |
| 1. Recognize Relevant Data | Assessment | Noticing | Recognize Cues |
| 2. Relationships Identified | Diagnosis/analysis | Interpreting | Analyze Cues Prioritize Hypotheses |
| 3. Respond to Current Priority | Planning Implementation | Responding | Generate Solutions Take Action |
| 4. Risks & Red Flags Identified | Not made visible | Not made visible | Not made visible |
| 5. Re-evaluate Patient’s Response | Evaluation | Reflecting in Action | Evaluate Outcomes |
| 6. Reflect & Refine Thinking | Not made visible | Reflecting on Action | Not made visible |
The 6 R’s of Clinical Reasoning is not meant to replace what you’re already using; it’s designed to strengthen it.
It aligns with the Nursing Process, Tanner’s CJM, and even the NCSBN Clinical Judgment Measurement Model. But it brings a practice-informed lens that highlights the importance of risk recognition.
Why Risk Recognition Matters
While risk anticipation is implied in the nursing process, as well as in Tanner’s and the NCSBN clinical judgment models, it’s not made clearly visible. Students are often taught to respond to the current problem, but not to prepare and anticipate for potential problems that could likely occur based on the reason patients are requiring care.
By explicitly including “Risks & Red Flags Identified” as a step in the reasoning process, the 6 R’s framework equips students to identify complications early and intervene before they escalate.
And that can mean the difference between life and death.
- How are you currently helping students identify and anticipate potential complications before they escalate?
- How could you intentionally integrate the 6 R’s of Clinical Reasoning into your teaching at each level?
Closing Thoughts
There’s still a gap between how nursing is taught and how it’s practiced, and it may be impacting our graduates’ successful transition to practice. By integrating a clinical judgment model, such as Tanner’s, into your curriculum, a nurse educator can use the 6 R’s of Clinical Reasoning teaching framework to operationalize it.
Despite the many challenges facing our profession and how it is taught, together we can bridge the gap by making the steps of clinical reasoning and risk recognition visible to students.
Related KeithRN Articles
How Do You Spell Clinical Judgment? T-A-N-N-E-R
Integrating Tanner’s Clinical Judgment Model in Your Teaching
References
- National Council of State Boards of Nursing. (2025, July). 2024 NCLEX® Examination Statistics (Vol. 94). Chicago, IL.
- Kavanagh, J. M. (2021). Crisis in Competency: A Defining Moment in Nursing Education. Online Journal of Issues in Nursing, 26(1).
- American Nurses Association. (2024). Registered nursing leaving the profession: Causes, consequences, and solutions. Online Journal of Issues in Nursing, 29(2). https://ojin.nursingworld.org/table-of-contents/volume-29-2024/number-2-may-2024/registered-nursing-leaving-the-profession/
- Nielsen, A., Gonzalez, L., Jessee, M. A., Monagle, J., Dickison, P., & Lasater, K. (2023). Current practices for teaching clinical judgment: Results from a national survey. Nurse Educator, 48(1), 7–12. https://doi.org/10.1097/NNE.0000000000001268
- Tanner, C. A. (2006). Thinking like a nurse: A research-based model of clinical judgment in nursing. Journal of Nursing Education, 45(6), 204–211.
Keith Rischer – Ph.D., RN, CCRN, CEN
As a nurse with over 35 years of experience who remained in practice as an educator, I’ve witnessed the gap between how nursing is taught and how it is practiced, and I decided to do something about it! Read more…
The Ultimate Solution to Develop Clinical Judgment Skills
KeithRN’s Think Like a Nurse Membership
Access exclusive active learning resources for faculty and students, including KeithRN Case Studies, making it your go-to resource.