Recently, a lively discussion erupted in our Teachers Transforming Nursing Education Facebook group after a tutor who works with nursing students asked:
“Has anybody noticed nursing schools adding a lot of extra ‘busy work’ in an attempt to help nursing students improve?
Students tell me they are assigned BOTH ATI and Elsevier modules, and they’re drowning in online assignments instead of learning to think like a nurse.”
Educators Weigh In
Dozens of educators had something to share. The conversation revealed not only differing opinions but a deeper tension in nursing education today.
On the surface, it’s about modules, readings, and active learning assignments.
But beneath it lies a critical question:
Are we truly equipping students for practice, or simply keeping them busy?
What Educators Are Seeing
There has been a trend away from traditional textbook reading toward an increase in supplemental modules and online assignments from various vendors. Many students perceive these tasks as “busy work”, activities that they feel are merely for the sake of completion rather than meaningful learning experiences.
I have noticed that whenever students are required to collaborate and do their part, such as through case-based active learning, they often label it as “busy work” and believe they are teaching themselves.
Educators, however, offered these observations:
- Many students lack essential study skills. Students often lack time management, organizational, and basic study skills to apply their learning. As a result, they focus on memorization and the “what” instead of deeply understanding the “why” of what they are studying.
- Reading Habits Have Changed. “Students don’t read textbooks anymore,” several instructors observed. Modules provide “cliff notes” that break complex content into digestible chunks and are interactive to engage students.
- Critical Thinking Gaps Are Real. New graduates struggle to develop adequate clinical reasoning and problem-solving skills. Faculty feel pressure to strengthen these skills before graduation.
But what are we doing to practice these critical thinking skills in our classrooms?
The Student Experience
While educators focused on the students and their struggles, though educators emphasized that what they assign is essential and meaningful, students often experience something different:
- Overload and Fatigue. When assignments pile up, students spend more time clicking through modules than reflecting, applying, or practicing their skills. Nursing education is often reduced to a series of tests and quizzes that must be completed successfully, while preparing students for practice takes a back seat.
- Disconnection. Without a clear explanation of HOW the nurse will use the content in any reading assignment, even well-designed activities feel like hoop-jumping to students. Something adult learners despise doing.
- Lost Opportunity for Deep Learning. Time spent “checking boxes” can crowd out and eliminate the time needed for application and active learning strategies such as simulation, authentic unfolding case studies and bedside application that have been shown to be best practices to build clinical judgment.
As one educator summarized, “Students are so busy completing modules that they don’t have time to actually practice thinking like a nurse.”
Busy Work vs. Purposeful Learning
The core tension is not the amount of work, because most students are willing to do the work, but the alignment and communication of that work and how it relates to nursing practice is often missing.
Assignments become “busy work” when:
- Their connection to clinical reasoning or patient care is unclear.
- Faculty cannot articulate why the activity matters.
- Students perceive the end goal as completing or passing the quiz, rather than as part of their professional transformation as a nurse to prepare them for practice.
The Trap of “More is Better”
Many educators admitted that accreditation and NCLEX pass rates influence their assignment decisions. Fear of poor program outcomes such as first-time NCLEX pass rates can create a “more is better” mindset:
“If some modules help, more modules must be even better.”
But as the blog by nurse educator Erin Putney, More is Better: Cognitive Bias in Education, reminds us, more does not equal better.
Volume of content can dilute value, overwhelming students and undermining deep learning.
Ironically, Jesus warned against this very tendency when He observed and challenged the behavior of the Pharisees, who added numerous burdens and obligations to the law that God never commanded in the Torah.
“You load people with burdens they can hardly carry” (Luke 11:46).
As nurse educators, we must be careful to ensure that our teaching lifts and equips our students, rather than crushing those we serve.
Lessons from the Facebook Discussion
Despite different experiences, several common strategies as solutions emerged from the conversation:
1. Align with practice.
Faculty who routinely review every assignment through the lens of practice readiness are trimming excess fat and focusing on what truly builds clinical judgment.
2. Communicate the Why.
Explaining the purpose of each assignment, linking it to patient care or safe nursing practice, changes how students perceive the workload.
3. Offer Flexibility.
Some instructors offer multiple learning options, enabling students to engage in ways that suit their learning style while achieving the same outcomes.
4. Prioritize Meaningful Active Learning.
Emphasize active learning that practices the thinking of practice such as simulation, case studies, and practice-based discussions, the very experiences that develop clinical judgment and practice readiness.
The transformation of nursing education occurs one nurse educator at a time, by changing the way you think about nursing education by prioritizing preparing students for practice.
Do this, and the NCLEX will take care of itself 🙂
How to Cut the Clutter
To make time for active learning in my classroom, I struggled to eliminate infobesity. However, as I reflected on essential knowledge and content from my lens of current nursing practice, a path to structuring assignments and classroom teaching became evident.
Check out our latest YouTube video that shares how any educator can transform the way nursing is taught.
You can download our handout, “Practice-Based Classroom Template,” which empowers nurse educators to streamline content to what is most important to nursing practice, eliminate information overload, and prioritize what matters most.
Reflection Questions for Educators
The transformation of nursing education begins with an honest self-examination by every nurse educator before assigning a reading or activity.
- Can I clearly explain the purpose of every assignment I give?
- Have I allowed accreditation or NCLEX pressures to drive my course design more than student learning that prepares them for practice?
- When students call something “busy work,” do I listen for valid concerns or dismiss their perspective by assuming they’re lazy?
- If I could start from scratch and do a course reset, what assignments would I keep, revise, or eliminate to focus on clinical reasoning and holistic, compassionate care?
We must never lose sight of the fact that patient care and human interaction remain foundational to holistic care. To learn how to integrate caring into your clinical teaching, see, Can Caring Be Taught on KeithRN.
Recommended Free Resources
 Free KeithRN Sepsis Clinical Reasoning Case Study
Free KeithRN Sepsis Clinical Reasoning Case Study
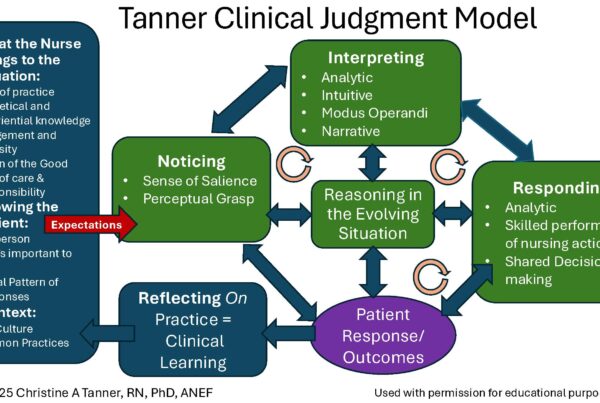
An easy-to-remember, practice-informed teaching framework based on Tanner’s Clinical Judgment Model that helps students identify risks to prevent failure to rescue to better prepare them for practice.
- Review your current course or next semester. Identify one or more assignments that could be simplified, better explained, or replaced with an authentic case study or simulation that uses open-ended clinical reasoning questions with no multiple-choice questions.
- Talk to your students. Ask them which activities most help them think more like a nurse. Be willing to ask them how they define busywork?
- Wisely consider their feedback. Listen carefully for common threads that may indicate an opportunity to revise or realign an assigned reading or activity.
- Pray for wisdom. Use your faith to guide and inform your implementation of teaching strategies. God promises that if you ask for wisdom, He will provide it (James 1:5). Seek God’s guidance to balance rigor with compassion, remembering that excellence in all you do honors Him.
Closing Thoughts
Let’s look at everything we do in nursing education through our lens of professional nursing practice. Let’s prioritize preparing students for practice by equipping them NEED to know content, not burdening or overwhelming them what is NICE, or even NUTS to know!
Remember that students still need educators who will emphasize the need to know content that guides them toward wisdom, critical thinking, and compassionate care, thereby equipping them to care for people and provide authentic, patient-centered, holistic care.
Let’s role model the values we want our students to demonstrate in practice: caring, compassion, integrity, and excellence anf commit to teaching with clarity, purpose, and passion, preparing students who are well prepared to serve as nurses and have a lasting career making a difference in all they do.
P.S. Join the conversation.
Ask your students how they define “busywork”? Their answers may surprise you!
What strategies have you used to eliminate busy work and prioritize preparing students for practice?
Share your thoughts in the Teachers Transforming Nursing Education Facebook group or in the comments below.
Keith Rischer – Ph.D., RN, CCRN, CEN
As a nurse with over 35 years of experience who remained in practice as an educator, I’ve witnessed the gap between how nursing is taught and how it is practiced, and I decided to do something about it! Read more…
The Ultimate Solution to Develop Clinical Judgment Skills
KeithRN’s Think Like a Nurse Membership
Access exclusive active learning resources for faculty and students, including KeithRN Case Studies, making it your go-to resource.



 6 R’s of Clinical Reasoning
6 R’s of Clinical Reasoning