Updated 8.12.2025 by Tiffany Condren, PhD, RNC, CHSE
Originally published 3.19.2020.
If you’re old enough to remember the iconic Rolaids commercial from the 1990s, you may recall the question: “How do you spell relief? R-O-L-A-I-D-S.” In the same way, nurse educators must ask a more urgent question: How do you spell clinical judgment? The answer is just as straightforward: T-A-N-N-E-R.
Why Tanner Still Matters
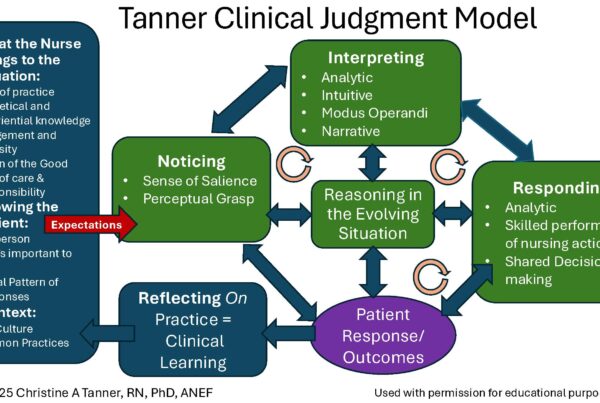
Chris Tanner’s model of clinical judgment, published in 2006 in the Journal of Nursing Education, remains the gold standard for understanding how nurses think, act, and make decisions at the bedside. Synthesizing findings from nearly 200 studies, Tanner laid out the foundational reasoning steps that underpin safe, effective nursing practice.
As the Next Generation NCLEX (NGN) raises the bar by evaluating clinical judgment explicitly, many educators can feel overwhelmed by complex frameworks and unfamiliar terminology.
But the good news is this: Tanner’s four-step model aligns seamlessly with NGN’s six-step process, offering a grounded and accessible pathway to prepare students for both licensure and real-world practice.
Just as the Rolaids commercial made its message simple, Tanner makes clinical judgment understandable and teachable by providing a clear, evidence-based framework that can be applied across all levels of nursing education.
Beyond Theory: Why It’s Urgent
Failure to rescue – when a nurse misses early signs of patient deterioration – is one of the most critical deficits in nursing care and a recognized core measure of quality. This often begins with missing subtle changes in a patient’s clinical condition, which leads to poor outcomes. Clinical reasoning is the key to preventing failure to rescue, and Tanner’s framework directly addresses this gap. It guides nurses to:
- Notice subtle changes from baseline.
- Interpret their clinical relevance.
- Respond appropriately and adapt as needed.
- Reflect to strengthen future judgment.
When applied consistently, these steps help prevent failure to rescue and improve patient outcomes. Faculty play a pivotal role by creating safe learning environments, modeling this reasoning process, and guiding students through repeated, scaffolded practice in both the classroom and clinical setting.
Who is Chris Tanner?
Chris Tanner, a professor at Oregon Health & Science University and longtime editor of the Journal of Nursing Education, articulated truths about nursing practice that remain powerfully relevant.
Her collaboration with Dr. Patricia Benner, one of the most influential voices in shaping nursing education’s approach to clinical judgment, further validates her influence in shaping how nurses are educated today.
How Tanner’s Four Steps Align with the NCSBN Clinical Judgment Measurement Model (NCJMM)
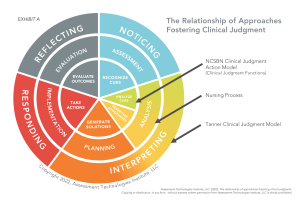 The NCSBN Clinical Judgment Measurement Model (NCJMM) is the assessment backbone of the Next-Generation NCLEX (NGN). While NCJMM is intended for evaluation – not instruction – its core steps mirror Tanner’s model:
The NCSBN Clinical Judgment Measurement Model (NCJMM) is the assessment backbone of the Next-Generation NCLEX (NGN). While NCJMM is intended for evaluation – not instruction – its core steps mirror Tanner’s model:
Recognizing this overlap allows educators to confidently teach using Tanner’s model while knowing students are also building the competencies assessed by NGN.
A Closer Look at Tanner’s Steps
- Noticing – More than just an “assessment,” noticing is a nurse’s ability to see what’s relevant, informed by patient history, prior interactions, and clinical experience. It’s the culmination of the nurse’s understanding of an individual patient’s baseline and typical responses. What is noticed—or missed—determines whether the correct nursing action will be taken. Active noticing requires recognizing and prioritizing relevant cues while filtering out noise. The nurse’s cognitive, metacognitive, and affective skills all influence what is noticed.2. Interpreting – Once cues are gathered, the nurse makes sense of them in context. This step is more than analysis—it involves sorting the information, prioritizing cues, generating multiple hypotheses, and anticipating possible complications. For new graduates, this is often the most challenging step because it demands applying classroom knowledge in a fast-paced, unpredictable bedside environment.
3. Responding – Here, judgment becomes action. The nurse selects and carries out interventions while adapting to rapid changes in the patient’s condition. This is where the integration of noticing and interpreting produces a safe, appropriate course of action, and the ability to adjust is critical to patient safety.
4. Reflecting – Reflection happens in two ways: in-action (while providing care, making adjustments as needed) and on-action (afterward, evaluating what worked and what didn’t). Both forms of reflection connect decisions with patient outcomes and deepen clinical judgment over time. Structured reflection during post-conference or debriefs strengthens learning and builds confidence.
From Classroom to Clinical: Making It Stick
To develop true clinical judgment, students need more than lectures and test prep. They need deliberate, consistent practice in both classroom and clinical settings with opportunities to apply the same reasoning process in both environments. This alignment helps students connect cognitive knowledge to applied clinical judgment.
Programs that intentionally align Tanner’s framework with curriculum design and pedagogy create a shared language among faculty and consistent expectations for students, helping them progress from novice to expert.
Application
Here’s how to bring Tanner’s model to life in your classroom, clinicals, and curriculum:
- Download and read Tanner’s seminal article, “Thinking Like a Nurse.”
- Integrate her four steps into every case, clinical post-conference, and class discussion:
- What do you NOTICE?
- How do you INTERPRET that data?
- How will you RESPOND?
- What did you REFLECT on?
- Use active learning strategies like unfolding case studies to give students repeated practice.
- Frame post-conference debriefs around the two types of reflection Tanner describes: in-action and on-action.
- Embed this model into your curriculum as a core theoretical framework.
 Key Takeaway Tanner’s model isn’t just another theory. It’s the clinical reasoning engine that drives safe, competent nursing care.
Key Takeaway Tanner’s model isn’t just another theory. It’s the clinical reasoning engine that drives safe, competent nursing care.
By teaching students to think like a nurse using Tanner’s four steps, we move beyond rote memorization toward true professional readiness. This addresses the most urgent patient safety issues, including failure to rescue, by giving nurses the tools to notice, interpret, respond, and reflect in a way that directly improve patient outcomes.
 PAUSE & REFLECT
PAUSE & REFLECT
Think about your own teaching practice. Are you unintentionally reinforcing passive learning through lectures and test prep? Or are you equipping students to recognize relevance, interpret meaning, take appropriate action, and reflect meaningfully?
Tanner gives us a mirror—and a roadmap.
Final Thoughts
Multiple ways of thinking are needed in nursing education, but Tanner’s model offers a bridge between classroom theory and bedside action. Let’s stop chasing the latest buzzword and instead return to what’s proven, practical, and profoundly effective.
By embedding Tanner’s model across your program, you create a unified faculty approach that ensures every student is on the path to safe, judgment-grounded practice. And yes, you prepare them for the NGN—not with fear, but with confidence.
Recommended Resources
- Thinking Like a Nurse: A Research-Based Model of Clinical Judgment in Nursing (Tanner, 2006)
- [KeithRN Case Studies that incorporate Tanner’s Model]
- Think Like a Nurse Membership Resources
References
Cappelletti, A., Engel, J. K., & Prentice, D. (2014). Systematic review of clinical judgment and reasoning in nursing. Journal of Nursing Education, 53(8), 453–458.
Condren T. (2025). Clinical Judgment Development Through Model-Based Reflection in Clinical Nursing Education. Nursing education perspectives, 10.1097/01.NEP.0000000000001430. Advance online publication. https://doi.org/10.1097/01.NEP.0000000000001430
Dickison, P., Haerling, K. A., & Lasater, K. (2019). Integrating the National Council of State Boards of Nursing clinical judgment model into nursing educational frameworks. Journal of Nursing Education, 58(2), 72–78. https://doi.org/10.3928/01484834-20190122-03
Jessee, M. A., Nielsen, A., Monagle, J., Gonzalez, L., Lasater, K., & Dickison, P. (2023). A national report on clinical judgment model use in prelicensure nursing curricula. Nursing Education Perspectives, 44(1), 4–10. https://doi.org/10.1097/01.nep.0000000000001062
Nielsen, A., Gonzalez, L., Jessee, M. A., Monagle, J., Dickison, P., & Lasater, K. (2023). Current practices for teaching clinical judgment. Nurse Educator, 48(1), 7–12.https://doi.org/10.1097/nne.0000000000001268
Tanner, C. A. (2006). Thinking like a nurse: A research-based model of clinical judgment in nursing. Journal of Nursing Education, 45(6), 204–211.
Relevant YouTube!
Here is a video on our YouTube channel, Think Like a Nurse, that emphasizes practical strategies to understand Tanner’s model of clinical judgment.
The Ultimate Solution to Develop Clinical Judgment Skills
KeithRN’s Think Like a Nurse Membership
Access exclusive active learning resources for faculty and students, including KeithRN Case Studies, making it your go-to resource.