In order to transform nursing education, Patricia Benner and the coauthors of Educating Nurses emphasized that nurse educators must contextualize nursing content to clinical practice so students can see why it is relevant.
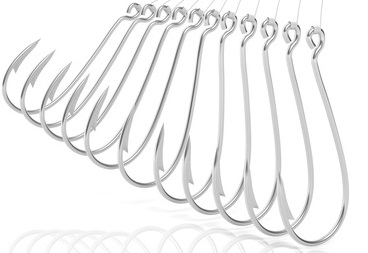
Lecture content must no longer be presented abstractly and regurgitated from the textbook alone. It must have a “hook” that contextualizes textbook content so it can literally be “caught” by students.
One of the greatest weaknesses of textbook learning is that it is linear. It can present only ONE topic at a time then go to the next. Real-world clinical practice is dramatically different. Patient care has become increasingly complex with three or more priority problems often presenting at the same time.
How can nurse educators effectively prepare students for this complex reality? By APPLYING the following THREE words that begin with the letter “C” from this short sentence:
CONTEXTUALIZE CONTENT through the use of CASE STUDIES!
Though case studies have been used for decades to teach any practice based profession such as nurses, physicians, and attorneys, this “old school” pedagogy is low cost and extremely effective to situate practice realities. It is another way to integrate simulation into your program, no high fidelity Sim-Man required!
To demonstrate this truth, I will take a scenario from an eating disorder case study I recently authored and provide just a small excerpt that highlights how case studies may be the “missing link” to transform your content and strengthen student learning!
The Case Study Begins…
Though this case has anorexia nervosa as the primary medical problem, the top three nursing concepts that are addressed in order of priority include:
- F&E
- Perfusion
- Nutrition
In order for a case study to be effective, it must be salient and accurately reflect real-world practice. This scenario was developed through the tragic themes of young women I cared for with eating disorders and the physical and mental health challenges they can represent.
History of Present Problem:
Mandy White is a 16-year-old adolescent who has struggled with anorexia nervosa since the age of 11. She admits to drinking several large glasses of water daily. Mandy has also been recently engaging in self injurious behavior (SIB) of cutting both forearms and thighs with broken glass causing numerous lacerations and scars. Mandy presents to the emergency department (ED) with increasing weakness, lightheadedness and a near syncopal episode this evening. She admits to inducing vomiting after meals the past three weeks. She is 5’ 5” and weighs 83lbs/37.7 kg (BMI 13.8). Mandy is reluctantly brought in by her mother and does not want to be treated. As the primary nurse responsible for the care of Mandy, you overhear her say to her mother, “I hate everything about me! I am so tired of living, I wish I were dead!”
But patients are more than a physical being, to provide holistic care, the nurse must also be aware and in tune with the emotional and even spiritual needs of each patient that is cared for. This is the personal and social history of Mandy that also must be filtered for clinical RELEVANCE:
Personal/Social History
Mandy was sexually abused by her step-father from the age of six to twelve. She confided what was taking place to her mother and lives with her mother who is now divorced. Mandy is sexually active and promiscuous. She uses the app Tinder to meet older men for anonymous sexual encounters when her mother is working.
Clinical Reasoning Begins…
Two primary components of clinical reasoning is the ability of the nurse to recognize what clinical data is RELEVANT and what are the resultant nursing PRIORITIES. Two simple questions must then be answered by students to hook content that emphasize recognizing RELEVANT data:
- What data from the histories are RELEVANT and has clinical significance to the nurse?
- What is the RATIONALE for the clinical data identified as relevant?
Patient Care Begins
Once relevant data is recognized, just as in practice the nurse obtains vital signs and nursing assessment:
Vital Signs:
- T: 96.2 F/35.7 C (oral)
- P: 50 (regular)
- R: 16 (regular)
- BP: 86/44 MAP: 58
- O2 sat: 99% room air
Nursing Assessment:
- APPEARANCE: Wearing oversized baggy shirt. Emaciated appearance with little subcutaneous body fat, breasts atrophied
- RESP: Breath sounds clear with equal aeration bilaterally, nonlabored respiratory effort
- CARDIAC: Pale-pink, cool & dry, 2+ bilateral pitting edema of feet and ankles, heart sounds regular with no abnormal beats, pulses weak, equal with palpation at radial/pedal/post-tibial landmarks, cap refill <3 seconds
- GI: Abdomen scaphoid, several 1 cm open ulcers present on oral mucosa that are also dry and tacky, soft and tender to gentle palpation in epigastrium, bowel sounds hypoactive and audible per auscultation in all four quadrants
- GU: Voiding without difficulty, urine clear/dark amber, she has not her menses the past 6 months
- SKIN: Numerous vertical old scars from SIB present on both forearms, has several recent vertical lacerations that are partial thickness on her left forearm, hair on head is thinning, skin is dry with lanugo body hair apparent on both arms
In order to clinically reason the nurse must also be able to grasp the “essence” of this scenario and identify the nursing priorities based on correctly interpreting all clinical data collected. Next questions…
- What are your nursing priority(ies)?
- What interventions will you initiate based on this nursing priority(ies)?
The physician orders lab panels and the following results are obtained:
Complete Blood Count (CBC:)
- WBC: 4.0
- Hgb: 9.8
- Platelets: 85
- Neutrophil %: 60
Basic Metabolic Panel (BMP:)
- Sodium: 132
- Potassium: 1.9
- Chloride: 88
- CO2 (Bicarb): 16
- Anion Gap (AG): 8
- Glucose: 60
- Calcium: 8.5
- BUN: 35
- Creatinine: 1.5
Misc. Labs:
- Magnesium: 1.2
- Phosphorus: 1.9
Just as in practice, the nurse must correctly interpret abnormal lab values and their clinical significance by asking the following questions:
- What lab values are relevant that must be recognized as clinically significant to the nurse?
- What is the RATIONALE for the clinical data identified as relevant?
- What interventions are required as a result of these abnormal lab values?
- Does your initial nursing priority or plan of care need to be modified in any way after obtaining these lab results?
- What are your current nursing priorities that will determine your plan of care?
The Power of the “Hook” of Clinical Contextualization
Fluid and electrolytes is difficult content that must be mastered by students in order to have a foundation to correctly interpret and UNDERSTAND the clinical significance of relevant lab values. It is NOT enough to memorize the “hypo” and “hypers” of the most common electrolytes!
Nurses must be able to not only recognize relevant abnormal labs, but situate knowledge to develop a lab “plan of care” of essential nursing assessments and interventions.
For example in this scenario, once the significance of a significantly depleted potassium and magnesium are recognized, the potential for cardiac arrhythmias including torsades de pointes become apparent and will result in specific interventions and assessments to proactively anticipate and respond to any potential change in status.
FREE Sepsis Case Studies!
I have a FREE download of the three different levels of clinical reasoning case studies I have designed on sepsis, a NEED to know topic for every nursing student as well as templates to create your own! Each case study provides needed practice of clinical reasoning and mirror how a nurse thinks in clinical practice.
See for yourself with no obligation! Simply click the button below:
Prepare Student’s for Practice
The primary purpose of every nurse educator is to prepare students for clinical practice.
That is why I did not include multiple choices in this case study but every question is open ended and requires a response. Last time I checked there are no multiple choice options in clinical practice either! You either know it or you don’t!
To transform nursing education, content must be contextualized to practice (Benner, Sutphen, Leonard, & Day, 2010). By using my clinical reasoning case studies or other active learning tools to provide this needed change, you will not only prepare students to pass the NCLEX®, but more importantly they will be well prepared for real-world clinical practice!
What do you think?
What have you found effective as a nurse educator to prepare students for practice?
Comment below and let the conversation begin!
References
Benner, P., Sutphen, M., Leonard, V., & Day, L. (2010). Educating nurses: A call for radical transformation. San Francisco, CA: Jossey-Bass.
Keith Rischer – Ph.D., RN, CCRN, CEN
As a nurse with over 35 years of experience who remained in practice as an educator, I’ve witnessed the gap between how nursing is taught and how it is practiced, and I decided to do something about it! Read more…
The Ultimate Solution to Develop Clinical Judgment Skills
KeithRN’s Think Like a Nurse Membership
Access exclusive active learning resources for faculty and students, including KeithRN Case Studies, making it your go-to resource.



